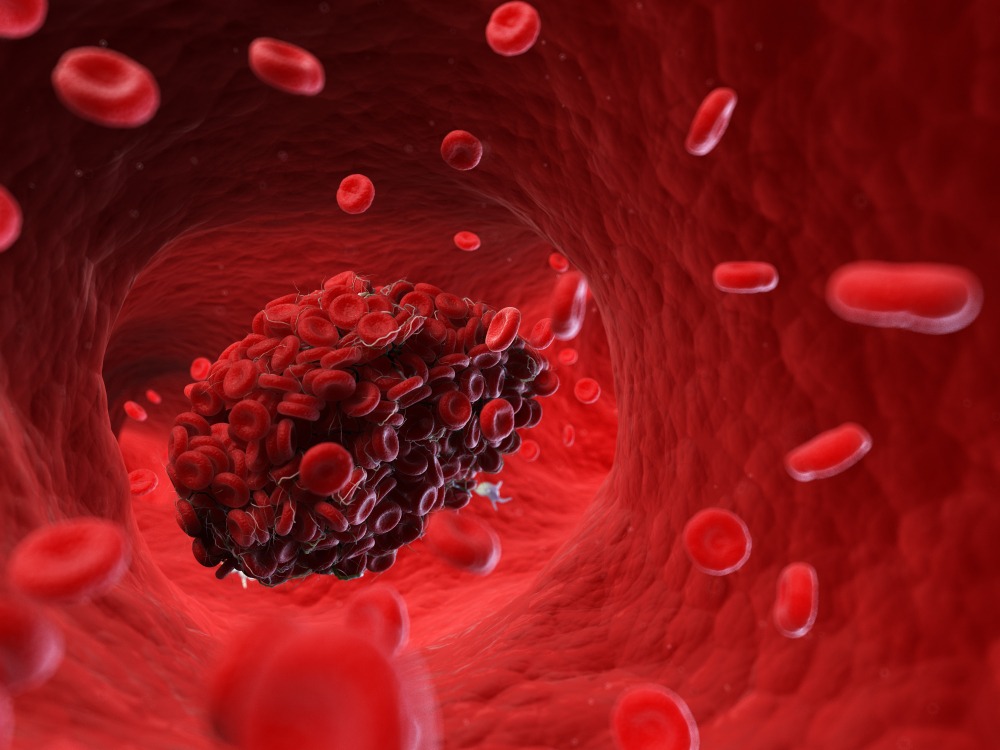
Your circulatory system, which propels blood throughout your body, is a work of art. But sometimes it can go awry and cause blood clots, which can be life-threatening. One specific type of blood clot that you’ve probably heard of—and maybe even worried about—is deep vein thrombosis (DVT).
DVT happens when blood clumps up in one of the veins deep inside your body, typically in your legs, according to the National Heart, Lung, and Blood Institute (NHLBI). Sometimes this kind of clot can dissolve without causing damage, but other times it can break off, travel to your lungs, and block blood flow. This is what’s known as a pulmonary embolism, and it can lead to organ damage or, in the most severe cases, even death.
Blood clots don’t always cause symptoms, but when they do, they’re likely to affect your legs. This is where clots tend to originate because gravity can cause blood to pool there, Sean Fischer, M.D., medical oncologist and hematologist at Providence Saint John’s Health Center in Santa Monica, California, tells SELF. You might experience swelling, cramping or soreness, red or discolored skin, or a feeling of warmth, according to the Centers for Disease Control and Prevention. If a blood clot travels to your lungs, it can cause shortness of breath, chest pain, dizziness or fainting, a rapid pulse, or even coughing up blood.
If you experience any signs of deep vein thrombosis or a pulmonary embolism, you need to seek medical attention immediately. With that said, it’s always good to brush up on knowledge of various health issues before one becomes a medical emergency. That’s especially true for blood clots, since there may actually be some steps you can take to prevent them.
There are only a few true causes of blood clots, but there are many risk factors that raise your odds of getting one—including some that you can change.
A model known as Virchow’s triad breaks down the three main causes behind blood clots. One is slower than usual blood flow, another is injury to a blood vessel, and the last is a genetic predisposition for clotting.
Various risk factors can contribute to these blood-clot causes. Some are non-modifiable risk factors, meaning you unfortunately can’t control them. But others are modifiable, as in, you can take steps to reduce your risk in these areas.
Below, you’ll find the most common risk factors for developing a blood clot. Identifying with one or even many of these doesn’t automatically mean you’ll wind up with blood clots, but it can be a sign that you should discuss your risk with your doctor.
1. Being pregnant or recently postpartum
Your estrogen levels rise when you get pregnant, and they stay elevated, increasing the odds that you’ll form a clot, Dr. Fischer says.
While blood clots can happen any time during pregnancy, the third trimester can be especially risky, Dr. Ross says, because most women move less during this period. And the risk doesn’t go away as soon as a person gives birth.
A 2014 study in the New England Journal of Medicine followed over 1.6 million women and found that in the first six postpartum weeks of every 100,000 deliveries, there were 22 clot-related health incidents. Seven to 12 weeks postpartum, that number was down to three cases out of every 100,000 deliveries. After that, the risk of a blood clot went back to what it was pre-pregnancy.
“Millions of women get pregnant and don’t have blood clots,” Natalie Evans, M.D., a vascular specialist at the Cleveland Clinic, tells SELF. However, having other risk factors on this list can increase your odds, so it’s important to discuss your full medical situation with your doctor, Dr. Evans says.
2. Being on combined hormonal birth control
Combined hormonal birth control uses estrogen and progestin to help prevent an unintended pregnancy. That’s typically a great thing, but estrogen in particular raises a person’s risk of DVT.
The mechanism behind this isn’t entirely understood, but it’s thought that estrogen increases the levels of certain clotting factors in your blood, according to the Mayo Clinic.
This is mainly a concern if you have certain risk factors like having a personal or family history of blood clots. Otherwise, your overall risk of developing a blood clot on birth control pills is low. According to a 2015 study in BMJ that looked at over 50,000 women, the chances of getting a blood clot while not on hormonal birth control are about 0.04 percent, then rise to 0.06 to 0.18 percent when on the pill, depending on the specific type. (The risk is higher on the contraceptive patch, which exposes people to 60 percent more estrogen than combined hormonal pills.)
The study also touched on the question of whether, when combined with estrogen, certain types of progestin can raise a person’s clot risk. While different types of progestin came with slightly different risks in this study, the definitive answer is still unclear. “The literature on this historically has shown that the estrogen component seem to be the driving factor with respect to thrombosis risk,” Dr. Fischer say, adding that “the mechanism behind this is not entirely understood” and more research needs to be done to determine how progestin affects blood clot risk with and without estrogen.
If you’re concerned about the hormones in your birth control raising your risk of blood clots, talk to your doctor about which method of contraception makes the most sense for you.
3. Sitting in a car, bus, or plane for long periods of time
When you travel for a long time, you might sit still for most of the journey, which can raise your risk of blood clots, according to the CDC. The longer you’re still, the greater your risk of developing a clot, Dr. Fischer says.
The CDC notes that moving your legs frequently and walking around every two to three hours can help lower your risk of developing DVT while traveling. You can even add on certain exercises, like extending your legs out and flexing your ankles, or ask your doctor if they have specific recommendations for how to lower your risk.
If you know you have other DVT risk factors, you may want to talk with your doctor before embarking on a long trip. They may suggest you use anticoagulants, wear compression stockings to keep blood from pooling in your legs, or take other steps to avoid blood clots.
4. Being overweight or obese
Having excess weight can put extra pressure on the lower half of your body, which can in turn increase the pressure in the veins there, according to the Mayo Clinic. Weight issues are incredibly complex, though, and this absolutely doesn’t mean that being overweight or obese guarantees that you’ll get DVT, Dr. Fischer says. Just like everything else on this list, your risk is intertwined with how many other risk factors you have.
5. Smoking
Lighting up damages a whole host of your body’s processes, and your circulatory system is no exception. Smoking can harm the lining of your blood vessels and also make it more likely that platelets in your blood will stick together, both of which can contribute to excessive blood clotting, according to the American Heart Association. But quitting smoking is usually easier said than done. Here are seven tips to get you started, and you can always ask your doctor for more specific advice. “It’s definitely worth quitting smoking for your overall health,” Dr. Evans says.
6. Being older
While people of any age can get a blood clot, the Mayo Clinic lists being older than 60 as one one of the major risk factors for developing DVT. The reasons for this aren’t well understood, Dr. Evans says. However, it may simply be that, as you get older, you’re more likely to develop other health conditions or illnesses that increase your risk of developing DVT, like cancer, Dr. Fisher says. It also may simply be that your blood has more potential to coagulate as you get older, he says. Still, there’s a lot of uncertainty around this one.
“Even healthy elderly patients are at higher risk of clots than their younger counterparts,” Dr. Evans says. “There is something about the biology of aging that increases clotting potential.”
7. Having surgery or getting injured
Surgery causes injury to your blood vessels, and in the process of your body trying to repair that vessel, a clot can form and travel, Dr. Fischer says. Lying in bed after an operation also increases your risk since you’re not moving as much. (This is why doctors generally recommend that you try to get up and be active as soon as medically advised after your operation.)
Given that most clots form in your lower extremities, having surgery on your hips or legs tends to put you at the greatest risk because your blood can easily slow or get stagnant down there post-op, Dr. Evans says.
Around four in 10 people who don’t receive medication to prevent blood clots will get DVT within one or two weeks of getting major knee or hip surgery, according to the U.S. National Library of Health. When you’re having surgery, be sure to ask your doctor what you can do to lower your risk of DVT, especially if you have other risk factors.
8. Having a clotting disorder
Some bleeding disorders, like hemophilia and idiopathic thrombocytopenic purpura (ITP), cause your blood to not clot enough. Others, like Factor V Leiden, fall on the opposite side of the spectrum. These can make your blood hypercoagulable, meaning it clots way too easily. While the symptoms vary by condition, if they do in fact lead to a blood clot or pulmonary embolism, you can expect typical symptoms like warmth, tenderness, redness, shortness of pain, a rapid heartbeat, and chest pain, according to the Mayo Clinic.
9. Having had DVT or pulmonary embolism in the past, or having a family member who has.
If you’ve experienced either of these conditions in the past, your doctor has likely advised you of your ongoing risk and how to keep it as low as possible. But having family members with DVT or pulmonary embolism is also a risk factor, according to the Mayo Clinic, so be sure to bring that up with your doctor if necessary.
10. Having inflammatory bowel disease
It sounds strange, but inflammatory bowel diseases like Crohn’s disease or ulcerative colitis raise your risk of getting a blood clot. A 2015 research paper in Thrombosis Journal says experts haven’t pinpointed a single cause behind why IBD can cause clotting issues but notes that people with these conditions may have genetic or immune abnormalities that can lead to difficulty with the coagulation process.
11. Having cancer or undergoing cancer treatment
Cancer also increases a person’s risk of having blood clots. “In general, the body’s clotting system gets exaggerated in people who have cancer,” Dr. Evans says. Specifically, various types of cancer may increase proteins that cause clotting, according to the American Heart Association.
So, you have one or more risk factors. What’s next?
Having a detailed conversation with your doctor about your concerns is a great step. They can help you figure out how to reduce your modifiable risk factors, like smoking and being inactive, Dr. Fischer says.
And if you suspect you have DVT or a pulmonary embolism, go to your local emergency room immediately. Doctors will examine you and run any tests necessary, then treat you with medications or procedures to break up the clot. These issues can be deadly when left untreated, so don’t hesitate to seek treatment—time is of the essence here.
Related: